What Is A Medial Branch Block?
A medial branch block is a treatment for pain that has developed due to a damaged or inflamed facet joint in the spine. A facet joint is a bony structure that connects spinal vertebrae together. Facet joints help control the movement of the spine and provide extra support and stability for the vertebrae. Clinical research has shown that facet joint pain is the cause of approximately 45% of all neck and back pain that is reported by patients.
Although facet joint problems are often the cause of neck and back pain, chronic pain may also be the result of trauma or an injury. Arthritis is another common condition that may affect the facet joints. It develops when cartilage that protects the joints begins to deteriorate or the synovial fluid that cushions them begins to decrease. Arthritis often occurs with age, but may also develop due to an autoimmune disease. Facet joint arthritis, in particular, may be a source of spinal irritation and back pain. Scoliosis, which is the abnormal curvature of the spine, and poor posture may also cause chronic back pain.
How Are Medial Branch Blocks Performed?
Steroid injections are a form of pain management treatment that is typically performed before a medical branch block is recommended. The injections involve the administration of an anesthetic (e.g., mepivacaine, bupivacaine, or lidocaine) as well as steroids (e.g., dexamethasome) directly into the region where the targeted facet joints are located. The injections usually provide patients with long-lasting pain relief. However, they are also used as a diagnostic tool to determine if a medial branch block will be effective. If two steroid injections produce dramatic pain relief, a physician will usually recommend the block procedure next.
A medial branch block is much more specific than a steroid injection and the effects generally last longer. The nerves that send sensory information to the facet joints (e.g., medial branch nerves) are targeted during the procedure. In order to block the nerve signals, a needle is inserted into the region where the affected nerves are located and then substances that destroy nerve tissue are administered. This causes the semi-permanent disruption of pain signal transmission and the significant relief of facet joint pain. Medical reports have shown that medial branch blocks are safe and effective for neck and back pain. This procedure is also quite beneficial in that it is non-invasive and helps patients avoid having to undergo surgery.
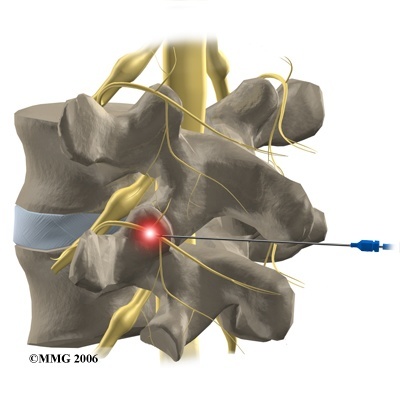
Risks that are associated with a medial branch block are generally related to problems with the needle placement or other technical errors. For instance, a small number of block procedures (approximately 3%) that were performed in the upper back or the neck resulted in the accidental injection of the medication into a blood vessel and not the targeted nerve. These types of complications are usually avoided, however, because the placement of the needle is guided by imaging devices such as an ultrasound, X-ray, or fluoroscope. When imaging technology is utilized during the procedure, the accuracy of needle placement is around 90%. Additional possible complications that may occur include bleeding at the injection site, nerve damage, and infection.
In addition to the administration of the substance that destroys nerve tissue, steroids and an anesthetic are also administered to the affected region. Possible side effects that may occur due to the steroids include weight gain, increased blood sugar levels, and even arthritis. The steroids may also weaken the immune system or cause stomach ulcers to form. The anesthetic that is injected may result in the gradual desensitization of healthy nerves and may also cause unwanted interactions with medication a patient may be taking. In an isolated number of cases, the injected anesthetic may cause nausea, chest discomfort, and temporary neurological problems. This has only actually occurred in approximately 2% of the patients who have received medial branch blocks. Due to the possible occurrence of such complications, physicians conduct thorough medical examinations before deciding if a patient is a good candidate for a medical branch block or not.
Conditions Related To Medial Branch Blocks
Diseases that affect the facet joints or injured joints in the neck (cervical region), the upper back (thoracic region), and especially the lower back pain (lumbar region) are often treated with medial branch blocks. The medication can be injected near vertebrae that have been directly affected by a particular injury or condition.
Watch this Review – Nerve Block Patient
Medial branch blocks in the lumbar region, effectively improve pain in the lower back and help approximately 40% of the patients regain their mobility. Most patients also report a reduction in pain of about 50% after treatment. Medial branch blocks in the cervical, lumbar, or thoracic region of the back are also effective diagnostic tools that help physicians assess the progression of certain spinal problems and whether or not a patient will need to undergo more invasive measures such as surgery.
Conclusion
A medial branch block is an effective form of pain management that reduces pain by disrupting damaged nerves in facet joints from transmitting signals to the brain. The block involves the injection of an anesthetic, steroids, and a substance that destroys nerve tissue. This combination of medication numbs the affected region, reduces inflammation, and hinders pain signal transmission.
Patients who undergo medial branch block procedures generally experience dramatic pain relief that may last for up to two years. The block procedure is also used as a diagnostic tool to confirm the location of affected facet joints.
References
- Jentzsch T, Geiger J, Konig MA, Werner CM. Hyperlordosis Is Associated With Facet Joint Pathology At The Lower Lumbar Spine. Journal of spinal disorders & techniques. Sep 27 2013 [Epub ahead of print]
- Lee HI, Park YS, Cho TG, Park SW, Kwon JT, Kim YB. Transient adverse neurologic effects of spinal pain blocks. Journal of Korean Neurosurgical Society. 2012;52(3):228-233.
- Verrills P, Mitchell B, Vivian D, Nowesenitz G, Lovell B, Sinclair C. The incidence of intravascular penetration in medial branch blocks: cervical, thoracic, and lumbar spines. Spine. 2008;33(6):E174-177.
- Kim D, Choi D, Kim C, Kim J, Choi Y. Transverse process and needles of medial branch block to facet joint as landmarks for ultrasound-guided selective nerve root block. Clinics in orthopedic surgery. 2013;5(1):44-48.
- Riew KD, Park JB, Cho YS, et al. Nerve root blocks in the treatment of lumbar radicular pain. A minimum five-year follow-up. The Journal of bone and joint surgery. American volume. 2006;88(8):1722-1725.
- Falco FJ, Manchikanti L, Datta S, et al. Systematic review of the therapeutic effectiveness of cervical facet joint interventions: an update. Pain physician. 2012;15(6):E839-868.
- Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V, Fellows B. The role of thoracic medial branch blocks in managing chronic mid and upper back pain: a randomized, double-blind, active-control trial with a 2-year followup. Anesthesiology research and practice. 2012;2012:585806.


